Many children are born with an underdeveloped tear-duct system, a problem that can lead to tear-duct blockage, excess tearing, and infection.
Blocked tear ducts are a fairly common problem in infants; as many as one third may be born with this condition. Fortunately, more than 90% of all cases resolve by the time children are 1 year old with little or no treatment. The earlier that blocked tear ducts are discovered, the less likely it is that infection will result or that surgery will be necessary.
What Are Tear Ducts?
Our eyes are continually exposed to dust, bacteria, viruses, and other objects that could cause damage. The eyelids and eyelashes play a key role in preventing these objects from entering our eyes and hurting them. But besides serving as barriers, the lids and lashes also help our eyes stay moist. Without moisture, our corneas, which serve as protective domes for the front of the eyes, would dry out and could become cloudy or injured.
Working with our lids and lashes, the protective system of glands and ducts called the lacrimal system keeps our eyes from drying out. Small glands at the edge of the eyelid produce an oily film that mixes with the liquid part of our tears and keeps them from evaporating. Lacrimal (or tear-producing) glands secrete the watery part of tears. These glands are located under the brow bone behind the upper eyelid, at the edge of the eye socket, and in the lids.
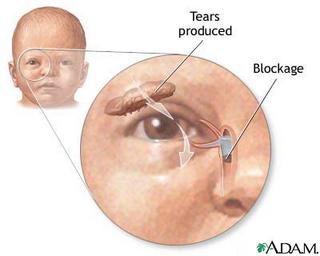
Eyelids move tears across the eyes. Tears keep the eyes lubricated and clean and contain antibodies that protect the eyes from infection. They drain out of the eyes through two ducts called punctum or lacrimal ducts, one on each of the upper and lower lids. From these ducts, tears enter small tubes called canaliculi, which are located at the inner corner of the eyelids. They pass from the eyes into the lacrimal sac, a small sac that's located next to the inner corner of the eyes (between the eyes and the nose).
From the lacrimal sacs, tears move down through the nasolacrimal duct and drain into the back of the nose. (That's why you usually get a runny nose when you cry - your eyes are producing excess tears, and your nose can't handle the additional flow.) When you blink, the motion forces the lacrimal sacs to compress, squeezing tears out of them, away from the eyes, and into the nasolacrimal duct.
The nasolacrimal duct and the lacrimal ducts are also known as tear ducts. However, it's the nasolacrimal duct that's involved in tear-duct blockage.
What Causes a Blocked Tear Duct?
Many children are born without a fully developed nasolacrimal duct. This is called congenital nasolacrimal duct obstruction or dacryostenosis. Most commonly, an infant is born with a duct that is more narrow than usual and therefore does not drain properly or becomes blocked easily. The majority of children outgrow this condition by the time they are 1 year old.
Less often, a child has a web of tissue over the end of the duct that didn't dissolve during fetal development. This condition is more likely to require surgical probing.
Other causes of blockage in children (especially older children) are rare. Some children have nasal polyps, which are cysts or growths of extra tissue in the nose at the end of the tear duct. A blockage also can be caused by a tumor in the nose, but again, this is unusual in children.
Trauma to the eye area or an eye injury that lacerates (cuts through) the tear ducts could also cause this condition, but reconstructive surgery at the time of the accident or injury may prevent blockage from happening.
Signs of Blocked Tear Ducts
Children with blocked tear ducts usually develop symptoms of the condition between birth and 12 weeks of age, although you may not realize your child has this problem until his or her eyes become infected. The most common signs of blocked tear ducts are excessive tearing, even when a child is not crying (this is called epiphora). You also may notice pus in the corner of your child's eye, or that your child wakes up with a crust over the eyelid or in the eyelashes.
Children with blocked tear ducts can develop an infection in their lacrimal sac called dacryocystitis. Signs of this infection include redness at the inner corner of the eye and a slight tenderness and swelling or bump at the side of the nose.
Another sign that the tear ducts may be blocked can be present at birth or soon after. Some infants are born with a swollen lacrimal sac, causing a blue bump called a dacryocystocele to appear next to the inside corner of the eye. Although this condition should be monitored closely by your child's doctor, it doesn't always lead to infection and can be treated at home with firm massage and topical antibiotics. However, if it becomes infected, the child is usually admitted to the hospital for intravenous antibiotics, followed by surgical probing of the duct.
When to Call Your Child's Doctor
If your child's eyes tear excessively but show no sign of infection, consult with your child's doctor or a pediatric ophthalmologist (eye specialist) to see if your child has a blocked tear duct. Early treatment can prevent the need for surgery. If your child shows signs of infection (such as redness, pus, or swelling), call your child's doctor immediately because the infection can spread to other parts of the face and the blockage can lead to an abscess if not treated.
Treating Blocked Tear Ducts
Children with blocked tear ducts often can be treated at home. Your child's doctor or pediatric ophthalmologist may recommend that you massage the eye several times daily for a couple of months. Before massaging the tear duct, wash your hands. Place your index finger on the side of your child's nose and firmly massage down toward the corner of the nose. You may also want to apply warm compresses to the eye to help promote drainage and ease any discomfort your child may have.
If your child develops an infection as a result of the tear-duct blockage, your child's doctor will prescribe antibiotic eye drops or ointment to treat the infection. It's important to remember that antibiotics will not get rid of the obstruction. Once the infection has cleared, you can continue massaging the tear duct as your child's doctor recommends.
If your child still has excess tearing after 6 to 8 months, develops a serious infection, or has repeated infections, the doctor may recommend that your child's tear duct be surgically probed. This procedure has an 85% to 95% success rate for children who are 1 year old or younger; the success rate drops as children age.
Surgical probing may be repeated if it's not initially successful. If your child continues to experience blockage, your child's doctor may recommend surgery to widen the tear ducts using tubes that are implanted in your child's tear ducts for 6 months, or a balloon that stretches the tear duct. Both of these surgical procedures have high success rates.
What Happens Before and During Surgery?
Surgery should be performed by a pediatric ophthalmologist who is familiar with the procedure - your child's doctor should be able to refer you to such a specialist. These surgical procedures are done on an outpatient basis (unless your child is suffering from a severe infection and has already been admitted to the hospital) under general anesthesia.
When a child is referred for a blocked tear duct because of an infection or excessive tearing, a pediatric ophthalmologist will do a complete eye exam to rule out any other eye problems or types of inflammation that might be causing similar symptoms.
A dye disappearance test also may help determine the cause of the problem. This involves placing fluorescein dye in the eye and then examining the tear film (the amount of tear in the eye) to see if it's greater than it should be. Or the doctor will wait to see if dye has drained properly by having the child blow his nose and then checking to see if any of the dye exited through the nose.
A surgical probe takes about 10 minutes. A thin, blunt metal wire is gently passed through the tear duct to open any obstruction. Sterile saline is then irrigated through the duct into the nose to make sure that there is now an open path. Infants experience no pain after the probing.
If surgical probing is unsuccessful, your child's doctor may recommend further surgical treatment. The more traditional form of treatment is called silicone tube intubation. In this procedure, silicone tubes are placed in your child's tear ducts to stretch them. The tubes are left in place for 6 months and then removed in another short surgical procedure. A newer form of treatment is balloon catheter dilation (DCP) or LacriCATH. In this procedure, a balloon is inserted through an opening in the corner of the eye and into the tear duct. The balloon is inflated with a sterile solution to expand the tear duct for 90 seconds. It is then deflated and reinflated for 60 seconds before being repositioned slightly higher in the duct and inflated twice again. It's then deflated and removed.
Both of these procedures require that your child be put under anesthesia and are fairly short - your child will be in surgery for less than an hour. Also, both procedures are considered to be generally successful. There is an approximate 80% to 90% success rate in younger children, with the chance of success decreasing if the procedure is done at older ages.
It may take up to a week after surgery before your child's symptoms improve. Your child's doctor will give you antibiotic ointment or drops along with specific instructions on how to care for your child.




2 comments:
Keep up the good work » »
This is very interesting site... »
Post a Comment